Brains!! I love brains. All other organs exist to supply the brain with oxygen and glucose. Fight me.
Anyway, I was thinking about brains and ICP, as one does, and decided to do a Nurse Files on it. I know brains seem complicated - and they can be - but most of neuro nursing is keeping the brain comfortable. Just the right pressure and temperature, the right stimulation, and the right nutrients. Get those balanced and you have some happy neurons!
Back to Basics
The Monroe-Kellie Hypothesis describes how the body compensates for changes in pressure and volume of the stuff inside your skull. It states, ‘the sum of volumes of brain, cerebrospinal fluid (CSF), and intracerebral blood is constant. Therefore, an increase in one component must be compensated by a decrease in one or both of the other components.’
Your skull is a fixed space. Once your fontanels close around 18-months of age, the volume inside your skull cannot expand except through normal growth rates. So, if there is sudden change in how much stuff is inside your skull, you need to compensate by reducing the others.
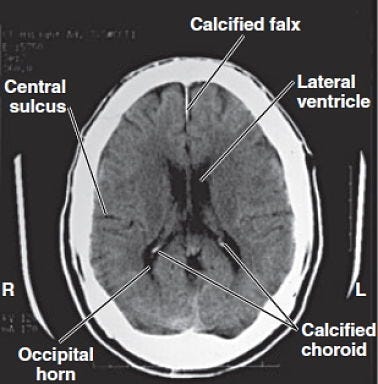
CSF - this is a water-based fluid. Your brain makes and absorbs CSF at a continual rate. You have special channels and ventricles that circulate CSF in and around your brain and spinal cord to keep everything clean and cushioned. It’s like the waterbed for your brain. CSF is the black areas of this CT:
Blood - is well, blood. It is supplied at a continual rate by the heart, maintaining an even blood pressure. You have receptors in your carotid arteries that are sensitive to pressure, carefully managing even the slightest changes in blood pressure with vasoconstriction and dilation. This ensures you have a steady supply of oxygen and glucose to feed the brain. Even a slight pause in supply will have you keeling over. The white areas on this CTA are the larger vessels. You can see the Circle of Willis: so cool!
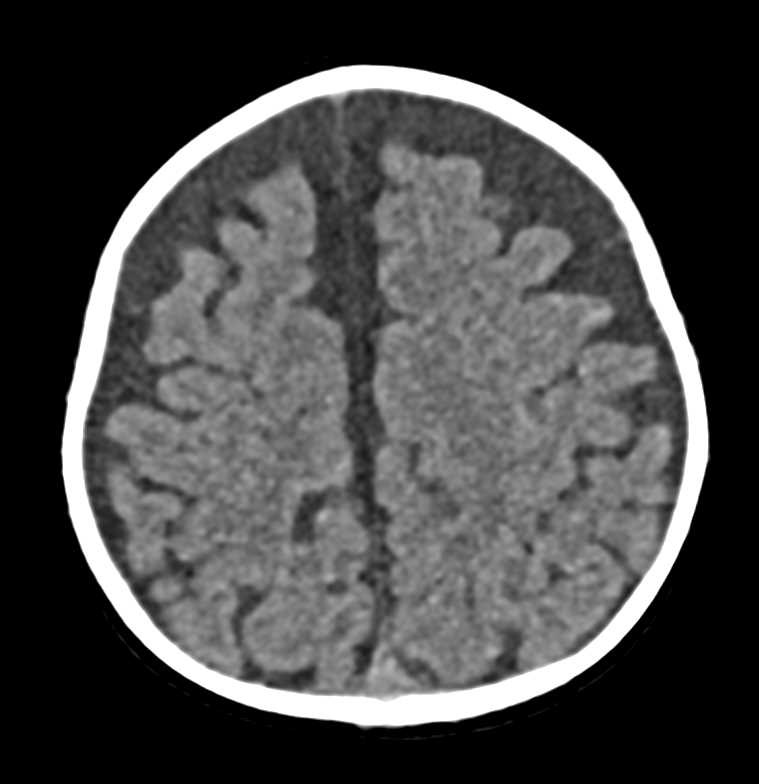
Brain Tissue - Your brain has a constant volume. It grows slowly as you reach maturity, stays steady for a while, and then slowly atrophies as you age. You can speed up this atrophy with poor health habits, like excessive alcohol consumption or methamphetamine use, but generally the shrinkage is small. Here’s a CT with significant atrophy. You can see all the empty space that should be brain has filled up with CSF. Bummer.
All these factors play into the Intracranial Pressure or ICP. Neuro ICU nurses care a lot about ICP. What it is, how its trending, what makes it go up and down. Everything in neuro-nursing comes back to ICP.
Bedside Considerations
To measure ICP directly, you have to drill a hole in someone’s skull. I’m not a huge fan of this unless it is absolutely necessary. There are significant complications if there is an infection or improper handling of the monitor and drain. Like, they die, complications. But there are times when this is a life-saving intervention. More on this in a minute.
When we don’t want/need a hole, but we want a good idea of what the ICP is doing, we can fall back on the Monroe-Kellie hypothesis and the body’s ability to autoregulate.
So, we have brain, blood, and CSF. Each has a normal volume that lives inside the skull. Blood and CSF are continuously moving around, but the volumes themselves stay relatively stable.
But what if they don’t? What if your patient forgets a dose of their blood pressure medicine and their pressure rises? Following the Monroe-Kellie hypothesis, one of the other substances will adjust to compensate.
Generally, this is the CSF. Resorption will increase, thus lowering the volume of CSF in the ventricles, reducing the ICP and maintaining equilibrium. As you may guess, brain volume is harder to adjust.
But it can change. When someone hits their head very hard and causes a concussion or contusion, the brain swells. Just like a sprained ankle, there will be 3-4 days of swelling, then reduction.
Unfortunately, you have that pesky skull. So, brain volume goes up and something else must come down. Again, CSF will be resorbed at a faster rate, but also the pressure inside the skull will force the blood out of the brain tissue.
But wait, we need blood in our brain, like every moment of every day. This is why head injuries can be so devastating. Your brain can swell so much, no blood can get inside. The brain can crush itself against the skull or herniate under and through the various hard structures of the skull. This is very, very bad.
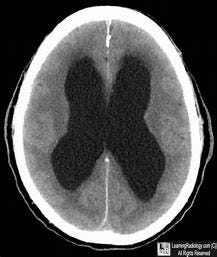
What if there is too much CSF? Perhaps the channels are blocked or something is interfering with resorption? You can get a brain that looks like this:
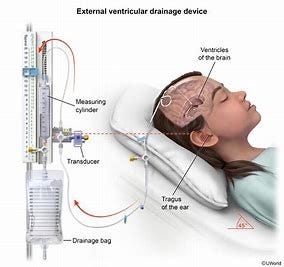
Oof. Can you see how the brain has been squashed? Brain tissue is actually pretty robust; it can be smooshed for a short time and expand again. I’ve touched a brain (and cut it into pieces) and I describe the consistency like a firm Jello mold. You can gently squash it and it won’t lose its integrity. But not for very long. Remember, you need blood to get into the tissue, which it can’t if the vessels are compressed. This person would need an extra ventricular drain ASAP and a shunt placed to divert excess CSF.
If my patient has one of these EVDs, don’t you dare touch them without my permission. I will chew you up and spit you out, I don’t care who you are. Too much CSF drained too fast and the patient’s brain will rip away from their skull and they will die. Too little drained and they can herniate and die. Don’t touch my patient.
Now, these are all worst-case scenarios. You know what else makes your ICP go up? Sneezing. Coughing. Bending down to tie your shoe. Rarely do these cause problems, because your brain is very good at regulating its ICP. It’s a princess, living large on a constant supply of O2 and glucose, and wants to stay there.
So, you sneeze. Even as you take a deep breath in preparation (and increase your thoracis pressure, thus your cerebral pressure), your body is shifting blood and CSF to allow for the increased pressure. Snot flies, eyes water, everything settles down, and barely the tiniest blip in your ICP.
Pretty awesome, right? Brains are the best.
References
Porth’s Pathophysiology: Concepts of Altered Health States (9th Edition). Grossman, S.C., Porth, C.M.
Wikipedia: Intracranial Pressure
Thank you for reading! You can follow me on Instagram and subscribe to this newsletter to stay up to date with posts, practice NCLEX questions, and my stories of life as an inpatient nurse.
If you found this article interesting, useful, or entertaining, please consider donating via a subscription. All This Is My Nurse Face content is free, but you can choose a subscription to help support my writing. My goal is to educate and inspire healthcare professionals and laymen alike. Your support helps me achieve that!
Also, please check out my other Substack: WritingRampant. No nursing, but occasional blood and guts. (My characters like to stab each other. Such drama queens...)
Enjoy!
Anna, RN, BSN, CCRN
Necessary disclaimer: I am discussing medications and medical conditions in this article based on my personal experiences as a nurse. Your facility may have different requirements and resources. Use your own nursing judgement to assess and treat your patients according to your governing body and facility guidelines. All information within this article is correct to the best of my knowledge, but should be confirmed through verified evidence-based sources. I am not responsible for any clinical decisions made based on this article.